Overview
Flat feet, fallen arches, or ?pes planus? is normally a symptomless and fortunately painless condition. It is characterized by the arch of the foot collapsing completely, which causes the entire sole of the foot to come into perfect contact with the ground. An estimated 20-30 percent of the entire population has some form of flat feet, ranging in severity from asymptomatic to somewhat problematic. Most people who endure this problem are able to experience life pain and symptom free from the nearly unnoticeable abnormality. However, a small sector of those affected do experience pain or discomfort, which is when a treatment program needs to be put in action.
Causes
Family history, experts say fallen arches can run in families. Weak arch, the arch of the foot may be there when no weight is placed on it, for example, when the person is sitting. But as soon as they stand up the foot flattens (falls) onto the ground. Injury, arthritis, tibialis posterior (ruptured tendon), pregnancy, nervous system or muscle diseases, such as cerebral palsy, muscular dystrophy, or spina bifida. Tarsal Coalition, the bones of the foot fuse together in an unusual way, resulting in stiff and flat feet. Most commonly diagnosed during childhood. Diabetes. Age and wear and tear, years of using your feet to walk, run, and jump eventually may take its toll. One of the eventual consequences could be fallen arches. The posterior tibial tendon may become weakened after long-term wear a tear. The postario tibial tendon is the main support structure of the arch of our feet. The tendon can become inflamed (tendinitis) after overuse - sometimes it can even become torn. Once the tendon is damaged, the arch shape of the foot may flatten.
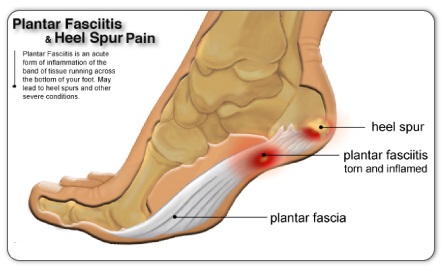
Symptoms
Having flat feet can be painless and is actually normal in some people. But others with flat feet experience pain in the heel or arch area, difficulty standing on tiptoe, or have swelling along the inside of the ankle. They may also experience pain after standing for long periods of time or playing sports. Some back problems can also be attributed to flat feet.
Diagnosis
An examination of the foot is enough for the health care provider to diagnose flat foot. However, the cause must be determined. If an arch develops when the patient stands on his or her toes, the flat foot is called flexible and no treatment or further work-up is necessary. If there is pain associated with the foot or if the arch does not develop with toe-standing, x-rays are necessary. If a tarsal coalition is suspected, a CT scan is often ordered. If a posterior tibial tendon injury is suspected, your health care provider may recommend an MRI.
fallen arches support
Non Surgical Treatment
What we want to do is support the arch and maintain it in that curved position. So what you want is to bring the foot into a position where you hold and support the arch so you can get that correct heel-midfoot-big toe contact. You would achieve that with a level of arch support. People will take different levels of support, if you?re somebody who has movement in your arch, a strong level of support will hold and maintain you whereas if you?re someone whose arch has collapsed it could need more support and a level of correction built into the support to realign you. If you think of it, when your arch drops, it affects your foot but it also has a biomechanical effect on the rest of the body. But nothing that can?t be solved.
Surgical Treatment

Fallen arches may occur with deformities of the foot bones. Tarsal coalition is a congenital condition in which the bones of the foot do not separate from one another during development in the womb. A child with tarsal coalition exhibits a rigid flat foot, which can be painful, notes the patient information website eOrthopod. Surgery may prove necessary to separate the bones. Other foot and ankle conditions that cause fallen arches may also require surgery if noninvasive treatments fail to alleviate pain and restore normal function.
Prevention
Donning a first-rate pair of arch supports, therapeutic socks and proper footwear before heading out to enjoy hours of holiday fun is one option to consider. Your podiatrist can help you find just the right ones. Once you have them on, they?ll help ease the amount of pressure being put on your body and keep the blood flowing in the right direction. While you?re standing in line, consider doing a bit of exercise as well. We?re not talking about channeling your inner Jack LaLanne here. Otherwise, you might attract the attention of the mall security guards. Simple ankle rotations and walking in place may help to reduce edema and give your flat feet a bit of a break. If you happen to be in a shopping mall or center where foot massages are available, take advantage of them periodically. They are likely to make you feel better and it?s a great excuse to carve out a few quiet moments for yourself. If you can?t visit a professional, tuck a personal foot massager into your purse. That way, you can lightly massage your own feet during the car ride home. Lastly, there are certain foods and nutritional supplements available that may reduce edema caused by standing on flat feet for hours at a time. The list includes potassium rich foods like raisins, bananas, baby carrots, nuts and yogurt. So, you may want to pack a snack for those trips to the mall or hit the food court before you hit the stores.
After Care
Time off work depends on the type of work as well as the surgical procedures performed. . A patient will be required to be non-weight bearing in a cast or splint and use crutches for four to twelve weeks. Usually a patient can return to work in one to two weeks if they are able to work while seated. If a person's job requires standing and walking, return to work may take several weeks. Complete recovery may take six months to a full year. Complications can occur as with all surgeries, but are minimized by strictly following your surgeon's post-operative instructions. The main complications include infection, bone that is slow to heal or does not heal, progression or reoccurrence of deformity, a stiff foot, and the need for further surgery. Many of the above complications can be avoided by only putting weight on the operative foot when allowed by your surgeon.
Flat feet, fallen arches, or ?pes planus? is normally a symptomless and fortunately painless condition. It is characterized by the arch of the foot collapsing completely, which causes the entire sole of the foot to come into perfect contact with the ground. An estimated 20-30 percent of the entire population has some form of flat feet, ranging in severity from asymptomatic to somewhat problematic. Most people who endure this problem are able to experience life pain and symptom free from the nearly unnoticeable abnormality. However, a small sector of those affected do experience pain or discomfort, which is when a treatment program needs to be put in action.
Causes
Family history, experts say fallen arches can run in families. Weak arch, the arch of the foot may be there when no weight is placed on it, for example, when the person is sitting. But as soon as they stand up the foot flattens (falls) onto the ground. Injury, arthritis, tibialis posterior (ruptured tendon), pregnancy, nervous system or muscle diseases, such as cerebral palsy, muscular dystrophy, or spina bifida. Tarsal Coalition, the bones of the foot fuse together in an unusual way, resulting in stiff and flat feet. Most commonly diagnosed during childhood. Diabetes. Age and wear and tear, years of using your feet to walk, run, and jump eventually may take its toll. One of the eventual consequences could be fallen arches. The posterior tibial tendon may become weakened after long-term wear a tear. The postario tibial tendon is the main support structure of the arch of our feet. The tendon can become inflamed (tendinitis) after overuse - sometimes it can even become torn. Once the tendon is damaged, the arch shape of the foot may flatten.
Symptoms
Having flat feet can be painless and is actually normal in some people. But others with flat feet experience pain in the heel or arch area, difficulty standing on tiptoe, or have swelling along the inside of the ankle. They may also experience pain after standing for long periods of time or playing sports. Some back problems can also be attributed to flat feet.
Diagnosis
An examination of the foot is enough for the health care provider to diagnose flat foot. However, the cause must be determined. If an arch develops when the patient stands on his or her toes, the flat foot is called flexible and no treatment or further work-up is necessary. If there is pain associated with the foot or if the arch does not develop with toe-standing, x-rays are necessary. If a tarsal coalition is suspected, a CT scan is often ordered. If a posterior tibial tendon injury is suspected, your health care provider may recommend an MRI.
fallen arches support
Non Surgical Treatment
What we want to do is support the arch and maintain it in that curved position. So what you want is to bring the foot into a position where you hold and support the arch so you can get that correct heel-midfoot-big toe contact. You would achieve that with a level of arch support. People will take different levels of support, if you?re somebody who has movement in your arch, a strong level of support will hold and maintain you whereas if you?re someone whose arch has collapsed it could need more support and a level of correction built into the support to realign you. If you think of it, when your arch drops, it affects your foot but it also has a biomechanical effect on the rest of the body. But nothing that can?t be solved.
Surgical Treatment

Fallen arches may occur with deformities of the foot bones. Tarsal coalition is a congenital condition in which the bones of the foot do not separate from one another during development in the womb. A child with tarsal coalition exhibits a rigid flat foot, which can be painful, notes the patient information website eOrthopod. Surgery may prove necessary to separate the bones. Other foot and ankle conditions that cause fallen arches may also require surgery if noninvasive treatments fail to alleviate pain and restore normal function.
Prevention
Donning a first-rate pair of arch supports, therapeutic socks and proper footwear before heading out to enjoy hours of holiday fun is one option to consider. Your podiatrist can help you find just the right ones. Once you have them on, they?ll help ease the amount of pressure being put on your body and keep the blood flowing in the right direction. While you?re standing in line, consider doing a bit of exercise as well. We?re not talking about channeling your inner Jack LaLanne here. Otherwise, you might attract the attention of the mall security guards. Simple ankle rotations and walking in place may help to reduce edema and give your flat feet a bit of a break. If you happen to be in a shopping mall or center where foot massages are available, take advantage of them periodically. They are likely to make you feel better and it?s a great excuse to carve out a few quiet moments for yourself. If you can?t visit a professional, tuck a personal foot massager into your purse. That way, you can lightly massage your own feet during the car ride home. Lastly, there are certain foods and nutritional supplements available that may reduce edema caused by standing on flat feet for hours at a time. The list includes potassium rich foods like raisins, bananas, baby carrots, nuts and yogurt. So, you may want to pack a snack for those trips to the mall or hit the food court before you hit the stores.
After Care
Time off work depends on the type of work as well as the surgical procedures performed. . A patient will be required to be non-weight bearing in a cast or splint and use crutches for four to twelve weeks. Usually a patient can return to work in one to two weeks if they are able to work while seated. If a person's job requires standing and walking, return to work may take several weeks. Complete recovery may take six months to a full year. Complications can occur as with all surgeries, but are minimized by strictly following your surgeon's post-operative instructions. The main complications include infection, bone that is slow to heal or does not heal, progression or reoccurrence of deformity, a stiff foot, and the need for further surgery. Many of the above complications can be avoided by only putting weight on the operative foot when allowed by your surgeon.



 If you sometimes feel that you are "walking on a marble," and you have persistent pain in the ball of your foot, you may have a condition called Morton's neuroma. A neuroma is a benign tumor of a nerve. Morton's neuroma is not actually a tumor, but a thickening of the tissue that surrounds the digital nerve leading to the toes. Morton's neuroma occurs as the nerve passes under the ligament connecting the toe bones (metatarsals) in the forefoot. Morton's neuroma most frequently develops between the third and fourth toes, usually in response to irritation, trauma or excessive pressure. The incidence of Morton's neuroma is 8 to 10 times greater in women than in men.
If you sometimes feel that you are "walking on a marble," and you have persistent pain in the ball of your foot, you may have a condition called Morton's neuroma. A neuroma is a benign tumor of a nerve. Morton's neuroma is not actually a tumor, but a thickening of the tissue that surrounds the digital nerve leading to the toes. Morton's neuroma occurs as the nerve passes under the ligament connecting the toe bones (metatarsals) in the forefoot. Morton's neuroma most frequently develops between the third and fourth toes, usually in response to irritation, trauma or excessive pressure. The incidence of Morton's neuroma is 8 to 10 times greater in women than in men.





 An Achilles tendon rupture, also known as an Achilles tendon tear, is the snapping or pulling apart of the Achilles tendon into two pieces. Achilles tendon ruptures can be full ruptures or partial ruptures. A physician may be required to distinguish between acute Achilles tendinosis and a partial Achilles tendon rupture. Tennis Leg is a rupture of the connection between the calf muscle and the Achilles tendon. Achilles tendonitis is an inflammation of the Achilles tendon: it is much less common than, but often confused with, Achilles tendinosis. Achilles tendons can also be lacerated or crushed.
An Achilles tendon rupture, also known as an Achilles tendon tear, is the snapping or pulling apart of the Achilles tendon into two pieces. Achilles tendon ruptures can be full ruptures or partial ruptures. A physician may be required to distinguish between acute Achilles tendinosis and a partial Achilles tendon rupture. Tennis Leg is a rupture of the connection between the calf muscle and the Achilles tendon. Achilles tendonitis is an inflammation of the Achilles tendon: it is much less common than, but often confused with, Achilles tendinosis. Achilles tendons can also be lacerated or crushed.
